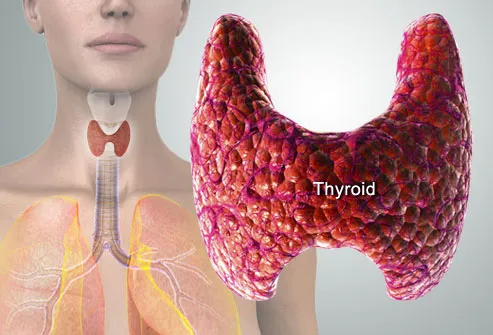
1- what is the vertical extension of the thyroid in relation to the vertebrae ?
a- C4 to T1
b- C5 to T1
c- C6 to T1
d- C3 to T1
answer : B
2- the thyroid develops from ?
a- ectoderm
b- mesoderm
c- dorsal pharyngeal gut endoderm
d- ventral pharyngeal gut endoderm
answer : D
3- screening method for medullary carcinoma of thyroid ?
a- serum calcitonin
b- serum calcium
c- serum ALP
d- serum acid phosphatase
answer : A
4- medullary carcinoma of thyroid arises from ?
a- parafollicular cells
b- cells lining the acini
c- capsule of thyroid
d- stroma of the gland
answer : A
5- which of the following is/are used in the management of thyroid malignancy?
a- Iodine 131
b- Iodine 125
c- Technitium 99
d- Phosphorus 32
e- strontium
answer is A
6- characteristic eye sign in dysthyroid status ?
a- exopthalmos
b- ptosis
c- optic neuropathy
d- myopathy
answer : A
7- hurthle cells are seen in ?
a- hashimoto's thyroiditis
b- follicular cell carcinoma
c- hurthle cell thyroid adenoma
d- all the above
answer is D
8- C cells populate which part of the lateral lobe of the thyroid ?
a- upper one-third of the lateral lobe of thyroid
b- middle one-third of the lateral lobe of thyroid
c- lower one-third of the lateral lobe of the thyroid
d- distributed equally all over the lateral lobe of the thyroid
answer :B
9- pick out the correct statements .
a- the external laryngeal nerve runs close to the superior thyroid artery .
b- the recurrent laryngeal nerve runs close to the inferior thyroid artery .
c- the external laryngeal nerve runs close to the inferior thyroid artery .
d- the recurrent laryngeal nerve runs close to the superior thyroid artery .
answer : both A and B are correct . ( so the surgeon has to be very careful while ligating those arteries, while performing thyroidectomy ).
10- treatment of medullary carcinoma of the thyroid with lymphnode metastasis?
a- subtotal thyroidectomy + radioiodine
b- subtotal thyroidectomy + radiotherapy
c- neartotal thyroidectomy + radioiodine
d- neartotal thyroidectomy + radiotherapy
e- total thyroidectomy + radiotherapy
answer : E
11- what is near total thyroidectomy ?
a- right lobectomy + isthmusectomy
b- left lobectomy + isthmusectomy
c- bilateral lobectomy with isthmusectomy
d- right lobectomy + isthmusectomy + left half lobectomy
e- right and left lobectomy
answer : D
12- papillary carcinoma of thyroid with bone metastasis is treated by?
a- subtotal thyroidectomy + radioiodine
b- subtotal thyroidectomy + radiotherapy
c- near total thyroidectomy + radioiodine
d- near total thyroidectomy + radiotherapy
e- total thyroidectomy + chemotherapy
answer : C and D
13- most common cause of thyroiditis is ?
a- hashimoto's thyroiditis
b- reidl's thyroiditis
c- subacute thyroiditis
d- viral thyroiditis
answer : A
14- thyroglossal cyst may occasionally give rise to which carcinoma ?
a- papillary
b- anaplastic
c- medullary
d- follicular
answer : A
15- a post-thyroidectomy patient develops signs and symptoms of tetany. The management is ?
a- I.V calcium gluconate
b- Bicarbonate
c- Calcitonin
d- Vitamin D
Answer : A
16- hypoparathyroidism following thyroid surgery occurs with in ?
a- 24 hours
b- 2-5 days
c- 7-14 days
d- 2-3 weeks
Answer : B
17- a patient undergoes thyroid surgery following which he develops perioral tingling . his blood calcium is 8.9 meq/l. next step in the management is ?
a- vitamin D orally
b- oral calcium and vitamin D
c- intravenous calcium gluconate and serial monitoring
d- wait for calcium to decrease to less than 7 meq/l before taking further action
answer : B
18- a patient after undergoing thyroid surgery presents with perioral paraesthesia . serum calcium level is 7 mg/dl . what will be the best management ?
a- oral vitamin D3
b- oral vitamin D3 and calcium
c- I.V calcium gluconate
d- Oral calcium
Answer : D
19- which of the following is not a complication of total thyroidectomy ?
a- bleeding
b- airway obstruction
c- hoarseness
d- hypercalcemia
answer : D
20- in post operative room after thyroid surgery , patient developed sudden respiratory distress , dressing was removed and it was found to be slightly blood stained and wound was bulging . what will be the first thing to be done ?
a- tracheostomy
b- cricothyroidectomy
c- laryngoscopy and intubation
d- remove the stitch and take the patient to O.T
answer : D
21- a patient presents with neck swelling and respiratory distress few hours after a thyroidectomy surgery. Next management would be ?
a- open immediately
b- tracheostomy
c- wait and watch
d- oxygen by mask
answer : A
22- after thyroidectomy patient developed stridor within 2 hours. All are likely causes of stridor except ?
a- hypocalcemia
b- recurrent laryngeal nerve palsy
c- laryngomalacia
d- wound hematoma
answer : A . hypocalcemia due to hypoparathyroidism after thyroid surgey normall results with in 2-5 days .
23- papillary carcinoma of the thyroid ( PCT ) patients are ?
a- euthyroid
b- hypothyroid
c- hyperthyroid
d- T3 thyrotoxicosis
Answer : A
24- HURTHLE cell carcinomas are derived from which cells ?
a- follicular cells
b- para follicular cells
c- oxyphilic cells
d- lymphocytes
answer : C
25- the malignancy which is common on long standing goiter ?
a- PCT
b- MCT
c- FCT
d- Anaplastic
Answer : C . Follicular carcinoma of the thyroid .
26- least malignant thyroid cancer ?
a- papillary
b- medullary
c- anaplastic
d- follicular
answer : a ( mean the more differentiation ) and the commonest tumor is it .
27- which of the following gene defects is associated with development of the medullary carcinoma of the thyroid ?
a- RET proto oncogene ( on chromosm 10 )
b- FAP gene
c- RB gene
d- BRCA 1 gene
Answer :A
RET proto gene : associated with medullary thyroid carcinoma, hirschsprung's disease and pheochromocytoma and rearrangement of RET gene leads to papillary thyroid carcinoma
28- psammoma bodies are seen in all of the following conditions except ?
a- serous cystadenoma of ovary
b- papillary carcinoma of thyroid
c- meningioma
d- mucinous cystadenoma of ovary
answer : D
29- all of the following are early life threatening complications of thyroid operation except ?
a- tracheomalacia and collapse of larynx
b- wound hematoma with compression of the trachea
c- hypocalcemia
d- thyroid storm
answer : C
30- in pregnancy ?
a- thiouracil is contraindicated
b- surgery is contraindicated
c- radioiodine is contraindicated
d- none
answer: C
31- lateral aberrant thyroid refers to ?
a- congenital thyroid abnormality
b- metastatic foci from primary in the thyroid
c- struma ovarii
d- lingual thyroid
answer : B
32- a patient presented with headache and flushing . he has a family history of his relative having died of a thyroid tumor. The investigation that would be required for this patient will be ?
a- chest x-ray
b- measurement of 5-HIAA
c- measurement of catecholamine
d- intravenous pyelography
answer : C . measurement of catecholamines . headache and flushing suggest symptoms of adrenal tumor and a history of thyroid tumor in the relative suggest the MEN syndrome type 2a or 2b . so the adrenal tumor is probably pheochromocytoma and so catecholamines have to be measured .
33- cancer that develops after irradiation ?
a- PCT
b- MCT
c- FCT
d- Anaplastic
Answer : A
34- mutated p53 gene is formed in most of ?
a- anaplastic carcinomas
b- PCT
c- MCT
d- FCT
Answer : A
35- treatment of choice for medullary carcinoma of thyroid is ?
a- total thyroidectomy
b- partial thyroidectomy
c- iodine 131 ablation
d- hemithyroidectomy
answer : A