An 11 year old male presents with fever up to 39 degrees (102 degrees F), joint pain and swelling, along with shortness of breath. The fever comes and goes at random times of the day. The symptoms have been present now for 4 days. Two days ago, his right knee was painful and swollen, but today it has improved. The joints involved today include the right ankle and left knee. They are quite tender, painful and also swollen. The shortness of breath occurs with walking, but he is now unable to walk because of the joint pain. He also has some shortness of breath with lying down flat when he is trying to sleep.
Examination:
VS T 38.2, P 160, RR 32, BP 100/60, oxygen saturation 94% in room air. He is tired appearing with tachypnea and tachycardia.
HEENT: Enlarged, erythematosus tonsils with exudates.
Lungs are clear but with tachypnea.
Heart sounds are tachycardic with a holosystolic murmur 3/6 heard at apex with radiation to axilla.
No gallops are heard. His PMI is prominent (size of silver dollar) at the 7th intercostal space in the mid-axillary line.
His abdomen is soft with normoactive bowel sounds. His liver edge is 6 to 7 cm below the RCM.
His left knee is swollen and extremely tender with warmth. He has difficulty with range of motion but can flex his knee 30 degrees passively. His right ankle is very swollen and warm. He has limited subtalar motion. Both his knee and ankle are very tender even to touch.
Neuro: No abnormal movements of arms, hands, or tongue are noted. He is unable to walk due to pain.
Clinical course:
The child is admitted to the hospital.
Initial laboratory work includes a erythrocyte sedimentation rate of 110, a CRP of 9.5, and a chest X-ray with cardiomegaly present.
EKG reveals a prolonged PR interval. ASO titer is 754 and streptozyme is 1:600.
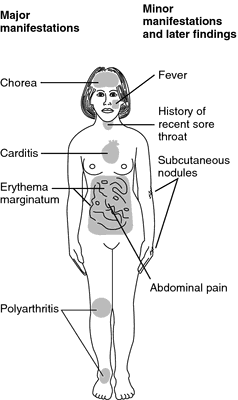
The diagnosis of acute rheumatic fever (ARF) is made and he is initially started on salicylate therapy at 75 mg/kg/day, and his arthritis improves dramatically.
However, the next day an echocardiogram confirms severe mitral insufficiency.
Due to the significant cardiac disease with elements of congestive heart failure he is switched to corticosteroids and improves.
His heart size decreases over the next 2 weeks, and when it normalizes he is switched back to salicylates for a total treatment duration of 8 weeks.
He does have a persistent murmur after this time however. He is started on intramuscular benzathine penicillin, which is given every 4 weeks for streptococcal prophylaxis.


0 comments:
Post a Comment